The Provider Claim Totals report lists all provider claims and includes meal counts and other data for that claim. The claim's Tier and the provider's current Tier (per effective dates in their file) are also included on this report.
Note: Claims that are on hold when this report is generated are not included in the report.
Each claim record is listed with its appropriate submission batch (Submitted Date). If a claim is marked as Not Yet, the claim has not been marked as submitted. If a claim is an adjustment claim, the value in the Status column is Adjustment. There can be as many adjustment claims for a given provider for a given month, but there should only be one original (core) claim.
The last page of this report contains summary total information, including the Total Homes Claiming and Total Unique Claims fields. These values will be different if a provider has more than one claim record in the given claim month.
The Total Zero-Dollar Homes Claiming field is also listed on the final page. While these providers are included in the Total Homes Claiming count, they should not be counted when reporting to the State, as your agency is not eligible for administrative funds for these providers. Subtract this number from your Total Homes Claiming when reporting a claiming home count to the State.
To print the Provider Claim Totals report:
- Click the Reports menu, select Claim Management, and click Provider Claim Totals Report. The Select Month dialog box opens.Notes: You can also print this report from the List Claims window. Click the Claims menu and select List Claims. Then, click Print. You can also click the Claims menu, select Submit Claims to State, and then click Print Provider Claim Totals. If you use this method, go to Step 7.
- Click the Select Month drop-down menu and select the claim month for which to print the report.
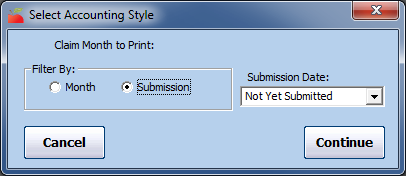
- Click Continue. The Select Accounting Style dialog box opens.
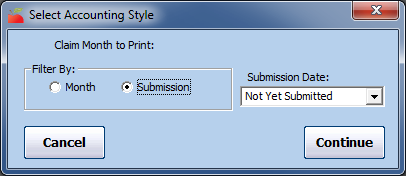
- In the Filter By section, select Month or Submission. If you select Month, go to Step 7.
- Click the Submission Date box and All Submission Batches or Not Yet Submitted. Not Yet Submitted is the default.
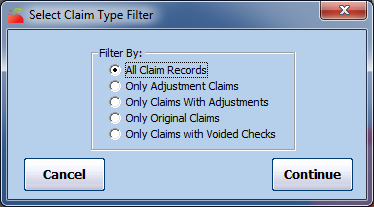
- Click Continue. The Select Claim Type Filter dialog box opens.
- Select the claim type by which to filter. In most states, this would be All Claims Records.
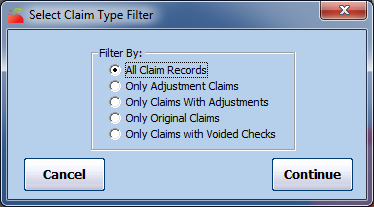
- Click Continue. The Provider Filter window opens. If you are printing this report from the Submit Claim to State window, go to Step 11 (the Provider Filter window does not display).
- Set additional filters for the providers to include in this report, if needed. If you don't set any filters here, all providers are included in the report.
- When finished, click Continue.
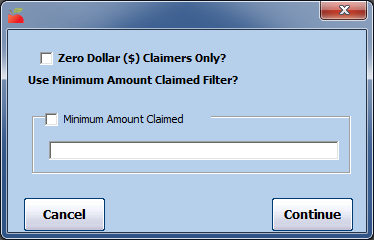
- You can now filter by claim dollar amounts, if needed. This can be useful if you're trying to isolate zero-dollar claimers (the entire claim was disallowed when processed). However, you should typically leave these filtering options un-changed when retrieving your state claim report information.
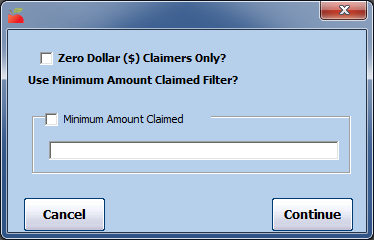
- Click Continue. The Provider Nested Sort Order dialog box opens.
- Click the First Sort By and the And Then By drop-down menus and select the primary and secondary sorts for this report.
- Click Continue. The report is generated.